How to Track Fatigue Without Getting Overwhelmed
Fatigue is sneaky. Some days it’s just life catching up to you; maybe you stayed up too late, had a stressful week, or skipped a few healthy meals. But other times, it’s a sign your body needs medical attention.
The tricky part? Fatigue can feel the same no matter the cause. That’s why tracking your symptoms can be so powerful: it helps you spot patterns, connect the dots, and decide when to make changes or seek medical help.
Lifestyle Fatigue vs. Medical Fatigue
A quick self-check:
- Lifestyle fatigue: Usually linked to things like poor sleep habits, long work hours, stress, or poor nutrition. Feels better after rest or a good night’s sleep.
- Medical fatigue: Sticks around even when you rest. You wake up feeling like you didn’t sleep at all.
If your sleep isn’t restorative, that’s a red flag to dig deeper.
Lifestyle Factors Worth Tracking
Sometimes fatigue isn’t a mystery illness; it’s your daily habits working against you. Here are questions you can track for a week or two:
Sleep:
- What time do you go to bed?
- How many times do you wake up during the night?
- What wakes you: heat, noise, pain, racing thoughts, needing to use the bathroom?
- How long does it take you to fall back asleep?
- How many hours of sleep do you need to function or feel rested?
Nutrition:
- Do you eat breakfast? Skipping it is a big cause of mid-morning energy crashes.
- Do you eat a lot of sugar and then crash an hour later?
- How much protein are you getting daily? (Many people eat less than they think.)
Daily energy flow:
- Do you have a regular mid-afternoon slump?
- When do you exercise, and how do you feel afterward: energized or wiped out?
Tracking these basics can reveal lifestyle fixes before you jump straight to medical testing.
Common Medical Causes of Fatigue
In my clinic, the most frequent causes I see include:
- Sleep issues: Insomnia, obstructive sleep apnea, or restless legs can keep you from getting deep, restorative sleep.
- Allergies: Constant nasal inflammation from allergic rhinitis can make you feel like you have a low-grade cold all the time and disrupt your sleep cycles.
- Autoimmune diseases: Chronic inflammation drains your energy even when you’re not active.
- Long COVID: Some people experience ongoing exhaustion, brain fog, and reduced stamina long after infection.
- Iron deficiency / anemia: Without enough hemoglobin, your body can’t carry oxygen efficiently.
- Depression: Low mood and low energy often go hand in hand.
- Low thyroid: Slows your metabolism so everything feels harder.
- Menopause: Hormonal changes can cause hot flashes, night sweats, and poor sleep.
Less common but important: POTS (a blood flow regulation problem) and ME/CFS (chronic fatigue syndrome).
Why “0–10” Fatigue Scales Don’t Work for Most People
Most medical fatigue scales were made for research, not daily life. They tell you “0 = no fatigue” and “10 = worst imaginable” but how do you actually decide between a 6 and a 7?
That’s why I made my own:
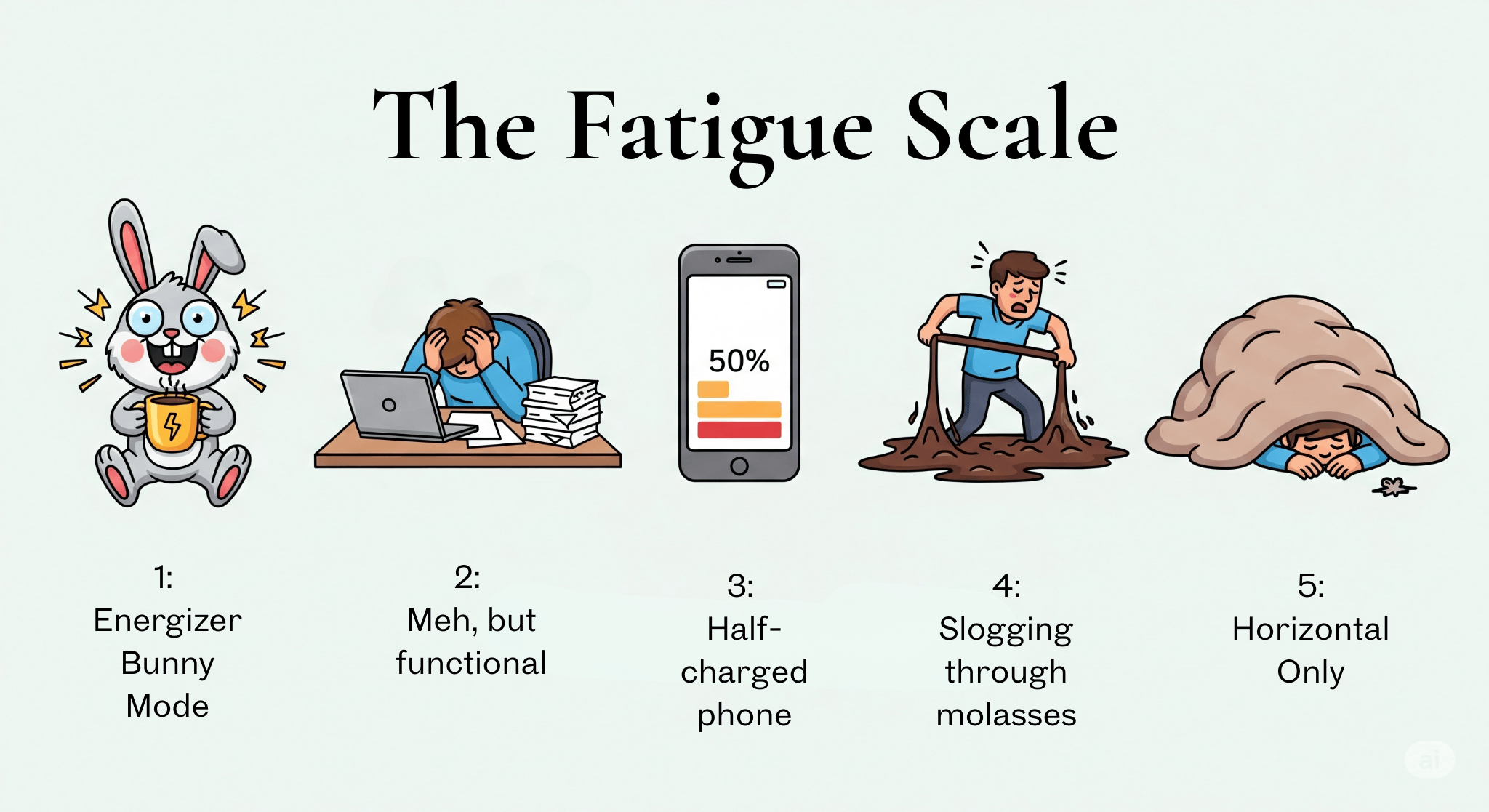
The Dr. G 1–5 Fatigue Scale
1️⃣ Energizer Bunny – You’re getting stuff done and might even socialize by choice.
2️⃣ Meh but Functional – You’ll get through the day, but dinner might be cereal.
3️⃣ Half-Charged Phone – You pick and choose what gets done. Laundry can wait.
4️⃣ Molasses Mode – Every task feels like wading through syrup. Showering is your workout.
5️⃣ Horizontal Only – The couch or bed is your home base. Brain fog is heavy.
How to Track Without Obsessing
You don’t need to record every detail of your life. In fact, over-tracking can make you more anxious. Here’s a sustainable way:
- Pick one fatigue score per day (morning, afternoon, or evening: just be consistent).
- Add 1–2 notes about context:
- Sleep details from the list above
- Big stressor, allergy flare, weather change
- Meals: especially breakfast, caffeine use, sugar crashes, or low protein days
- Exercise and how you felt afterward
- Review weekly, not hourly. Look for patterns like:
- Fatigue always worse on nights after poor sleep
- Energy dips after certain foods or skipped meals
- Fatigue stays high despite good sleep: that’s a reason to get checked for medical causes
Making Decisions from Your Tracker
Your tracker isn’t just for your doctor, it’s for you, too. Patterns can help you:
- Plan your week: If you always crash on Wednesdays, schedule lighter tasks or rest then.
- Spot triggers: Notice fatigue after certain meals? Time to review nutrition or check labs.
- Advocate for yourself: Instead of saying “I’m tired all the time,” you can say, “For the past 6 weeks, I’ve had level 4 fatigue, (feeling like I’m slogging through molasses) at least 4 days a week despite 8 hours of sleep.” That’s data a provider can work with.
Bottom line: Fatigue is complicated, but tracking doesn’t have to be. A simple daily score plus a couple of context notes can reveal patterns you’d otherwise miss; and help you take the next step toward feeling better.
I’ve made a free Weekly Symptom Tracker you can download to start today.
And if you’ve ever left a doctor’s appointment feeling dismissed or unheard, my last blog post shares 10 phrases you can use to make sure your concerns are taken seriously. You can read it here →
